Summary: Fat entering the intestines triggers a signal that is transmitted through neurons and to the brain, creating a desire for fatty foods.
Font: Columbia University
A dieter struggling with cravings for fatty foods might be tempted to blame their tongue: the delicious taste of butter or ice cream is hard to resist. But new research investigating the source of our appetite has uncovered an entirely new gut-brain connection that drives our desire for fat.
At Columbia’s Zuckerman Institute, scientists studying mice found that fat entering the intestines activates a signal. Conducted along the nerves to the brain, this signal generates a desire for fatty foods.
Posted on September 7, 2022 in NatureThe new study raises the possibility of interfering with this gut-brain connection to help prevent unhealthy choices and address the growing global health crisis caused by overeating.
“We live in unprecedented times, in which excessive consumption of fats and sugars is causing an epidemic of obesity and metabolic disorders,” said first author Mengtong Li, Ph.D., a postdoctoral researcher in the Charles Zuker lab of the Institute Zuckerman. Ph.D., supported by the Howard Hughes Medical Institute.
“If we want to control our insatiable desire for fat, science shows us that the key conduit that drives these cravings is a connection between the gut and the brain.”
This new view of dietary choices and health began with earlier work by the Zuker lab on sugar. The researchers found that glucose activates a specific gut-brain circuit that communicates with the brain in the presence of gut sugar.
No-calorie artificial sweeteners, by contrast, don’t have this effect, which likely explains why diet soda can leave us feeling unsatisfied.
“Our research shows that the tongue tells our brain what I like itlike things that taste sweet, salty or fatty,” said Dr. Zuker, who is also a professor of molecular biochemistry and biophysics and of neuroscience at Columbia’s Vagelos College of Physicians and Surgeons.
“The gut, however, tells our brain what wantWhat we need.”
Dr. Li wanted to explore how mice respond to dietary fats – the lipids and fatty acids that every animal must consume to provide the building blocks of life. He offered mice bottles of water with dissolved fats, including a soybean oil component, and bottles of water containing sweet substances that are known not to affect the gut but are initially appealing.
The rodents developed a strong preference, over a couple of days, for fatty water. They formed this preference even when scientists genetically modified mice to remove the animals’ ability to taste fat with their tongues.
“Even though the animals couldn’t taste the fat, they were driven to consume it,” Dr. Zuker said.
The researchers reasoned that fat must be activating specific brain circuits that drive the animals’ behavioral response to fat. To look for that circuit, Dr. Li measured brain activity in mice while he fed the animals fat.
Neurons in a particular region of the brainstem, the caudal nucleus of the solitary tract (cNST), perked up. This was intriguing because cNST was also implicated in the lab’s earlier discovery of the neural basis of sugar preference.
Next, Dr. Li found the lines of communication that carried the message to the cNST. Neurons in the vagus nerve, which links the intestine to the brain, also hummed with activity when the mice had fat in their intestines.
Having identified the biological machinery underlying a mouse’s preference for fat, Dr. Li then took a closer look at the intestine itself: specifically the endothelial cells that line the intestines. He found two groups of cells that signaled vagal neurons in response to fat.
“A group of cells functions as a general sensor for essential nutrients, responding not only to fat, but also to sugars and amino acids,” said Dr. Li. “The other group responds only to fat, which could help the brain distinguish fat from other substances in the gut.”
Dr. Li then took a further important step by blocking the activity of these cells with a drug. Shutting down signaling from either group of cells prevented the vagal neurons from responding to fat in the intestines. He then used genetic techniques to turn off the vagal neurons themselves or the neurons in the cNST. In both cases, one mouse lost its appetite for fat.
“These interventions verified that each of these biological steps from the gut to the brain is critical to an animal’s response to fat,” said Dr. Li.
“These experiments also provide novel strategies for changing the brain’s response to fat and possibly behavior toward food.”
The stakes are high. Obesity rates have nearly doubled worldwide since 1980. Today, almost 500 million people have diabetes.
“The overconsumption of cheap, highly processed foods high in sugar and fat is having a devastating impact on human health, especially among low-income people and in communities of color,” said Dr. Zuker.
“The better we understand how these foods hijack the biological machinery that underlies taste and the gut-brain axis, the more opportunities we have to intervene.”
Scott Sternson, Ph.D., a professor of neuroscience at the University of California, San Diego, who was not involved in the new research, highlighted its potential to improve human health.
“This exciting study provides insight into the molecules and cells that compel animals to crave fat,” said Dr. Sternson, whose work focuses on how the brain controls appetite.
“Researchers’ ability to control this craving may eventually lead to treatments that can help fight obesity by reducing consumption of high-calorie, fatty foods.”
About this research news in neuroscience and gut-brain axis
Author: press office
Font: Columbia University
Contact: Press Office – Columbia University
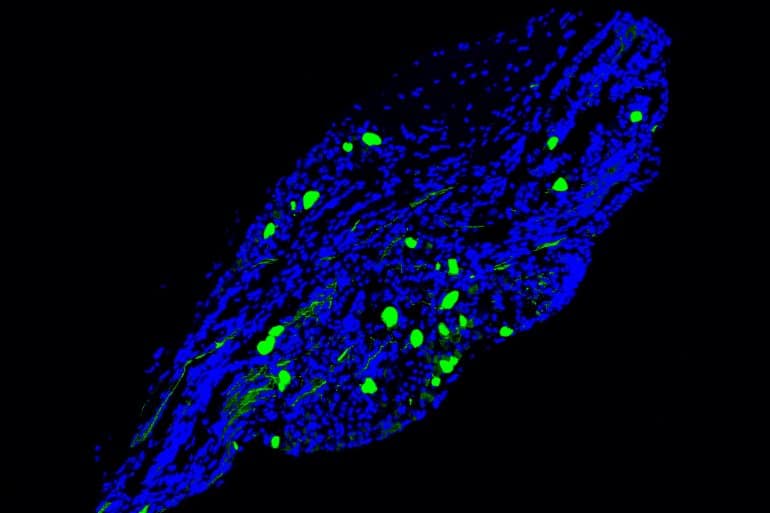
Image: Image is credited to Mengtong Li/Zuker lab/Columbia’s Zuckerman Institute
original research: Closed access.
“Gut-brain circuitry for fat preference” by Mengtong Li, Hwei-Ee Tan, Zhengyuan Lu, Katherine S. Tsang, Ashley J. Chung, and Charles S. Zuker. Nature
Summary
Gut-brain circuitry for fat preference
The perception of fat evokes strong appetitive and consummatory responses. Here we show that fat stimuli can induce behavioral attraction even in the absence of a functional taste system. We show that fat acts after ingestion through the gut-brain axis to drive preference for fat.
Using single-cell data, we identified vagal neurons that respond to intestinal fat delivery and showed that genetic silencing of this gut-to-brain circuit abolished the development of fat preference.
Next, we compared the gut-to-brain pathways that drive preference for fat versus sugar and uncovered two parallel systems, one functioning as a general sensor for essential nutrients, responding to gut stimulation with sugar, fat, and amino acids, while that the other is activated only by fatty stimuli.
Finally, we engineered animals that lacked candidate receptors for detecting the presence of intestinal fat and validated their role as mediators of gut fat-elicited responses to the brain.
Together, these findings revealed distinct cells and receptors that use the gut-brain axis as a critical conduit for the development of fat preferences.