But, in April this year, a phone call from a familiar voice forced Jha to break from her busy routine. ”Please come over, I need to talk,” the caller requested. ”It has to be you.”
On the line was Mamta Kumari, whom Jha had helped to climb out of a dark depression during her first full-term pregnancy in 2018. Jha made a mental note to visit Kumari when she had a spare moment.
She was no longer working for the mental health initiative and had enough else to do. But the calls kept coming and Kumari’s pleas grew more frantic and accusatory, Jha recalls. “You don’t have the time for us anymore,” the mother of two would start saying before reverting to supplications for help, the two women told CNN.
Days later, feeling a little guilty, Jha put on her helmet and rode her trusty red scooter the two kilometer distance from her house to Kumari’s house. She parked on the corner of a mud road a few minutes away, remembering that the rest of the journey would have to be done on foot through corn fields into the Ram Tola settlement in Nagargama village.
Once inside the house, Jha was introduced to a young pregnant woman, Anjali Kumari. Even before Kumari began to describe her sister-in-law’s condition, Jha had known instantly that something was amiss. She had been trained to recognize the signs.
”Anjali is four months pregnant, not eating properly for days on end, locking herself in a room, crying and getting agitated at the drop of the hat – she is just not her usual self,” Kumari explained to Jha, whispering so that other family members would not hear, both women recalled.
Kumari was gravely concerned because she too knew these behaviors well. This had been her four years ago, she said, desperately sad and losing weight.
Back then though, things had been different. Kumari had found out about, and was able to call, a local hotline that offered mental health advice to pregnant women and new mothers. It was through the hotline initiative that she had been connected to Jha, whom she now wanted to help her sister-in-law.
There was just one problem: Jha no longer worked on the hotline – no one did. Funding for this innovative mobile-based service had run out.
“If only we had some resources,” Jha remembers thinking, “I could have helped her get better.”
The hotline that became a lifeline
“Welcome to Samya Mobile Baani… which runs 24/7 and is also free of cost.”
“If you are stressed or want to talk about something, you can talk to our counselor by pressing 9.”
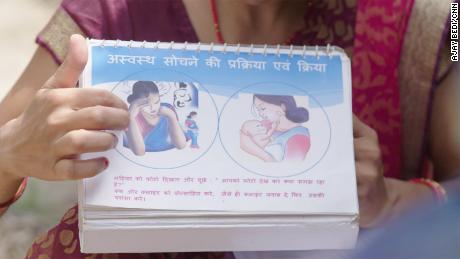
Everyone who called the hotline number was offered two options: listen to pre-recorded messages, skits or songs about maternal mental wellbeing or talk to a counselor. Some callers, such as Kumari, were also provided with the option of receiving talk therapy sessions at home.
Jha and 14 other locals on the payrolls of IIH were given training in community mental health, the basics of cognitive behavioral therapy and counseling. They were also given guidance on how to engage women in the villages to let them know about the hotline and help them open up about their difficulties. While two of the 15 would manage the calls, the rest would go door-to-door, offering counseling services.
Married in 2010, at the age of 15, Kumari became pregnant for the first time the following year but miscarried. Over the next eight years, she would have two more miscarriages and be put on treatment for an infection in her uterus, she told CNN.
As she processed the trauma of multiple miscarriages, Kumari told CNN she faced verbal abuse from the family. She said she began sewing clothes for money, hoping that the income she brought into the family would help her in-laws see her value.
A month after her third miscarriage, Kumari remembers becoming so lethargic that she struggled to sew, or even complete her daily chores. She went to her doctor who delivered the news: she was pregnant again.
Panic set in. Her latest pregnancy was labeled ‘high risk’ and Kumari became consumed with dread that she would soon lose another baby.
Her community health worker told the then 23-year-old about the new hotline. Uncertain but with nothing to lose, Kumari rang the number.
At the same time, the health worker alerted the IIH team rolling out the hotline of Kumari’s high-risk pregnancy, resulting in Jha arriving at Kumari’s door with a questionnaire to assess her mental health. This identified the young woman as being in urgent need of counseling, and soon her sessions with Jha began.
Providing at-home therapy threw up its own challenges in a poor rural community where people lacked awareness of maternal mental health, the vocabulary to explain what they were going through, or – often as women – the freedom and privacy to speak their mind.
“In regions such as ours, you can’t really walk into a house which has at least 10-12 people and say I am here to provide therapy to your daughter-in-law or wife.” Jha explained. “We had to keep the baby at the center.” When the family members are convinced that “we have entered their homes to ensure the well-being of the newborn or the fetus, then they would leave us alone with the women.”
In fact, Kumari herself could not understand why Jha wanted to talk to her about her feelings when they first met. No one had ever asked her about them before, she explained. It took three sessions, Jha recalls, for Kumari to start talking to her about her fears and tribulations. The sessions took place away from her family inside her small, dark sewing space.
But once she started opening up, the words came pouring out, Jha recalled, and Kumari revealed that she was petrified of losing another baby. She was worried about which foods could affect her pregnancy and so, had stopped eating completely, according to Jha.
“It took me a while to convince her to eat because she felt too dejected to eat and too nauseous to chew,” said Jha. “I explained how nutrition is important for the growth of the baby.”
Kumari began to eat again. Outside of her hour-long sessions with Jha which happened every 15 days, she found herself relying increasingly on the hotline’s recorded messages of advice and encouragement and the immediate access she could have to a counselor when in urgent need of solace. “It made me feel good,” she told CNN.
Kumari saw that pregnancy safely to term and says she continued to practice the habits learned from the Samya Mobile Baani hotline and team: drink a glass of water whenever you feel angry; start meditating whenever you feel helpless and ensure you are eating healthily.
”When I became pregnant again in late 2020, I just remembered what Jha had told me during my pregnancy in 2018 and kept following her advice. And that is why my last pregnancy went so smoothly,” Kumari said, her voice full of confidence.
Women ‘do not have any agency’
Depression during pregnancy or in the first year after giving birth (known as perinatal depression) is one of the most common mood disorders affecting women worldwide. It differs from postpartum depression in that it includes the period before and not just after the baby is born.
The risk factors for perinatal mental health disorders in this part of the world are in part the pressures and hardships of being a woman, explained Homam A. Khan, a program manager at IIH who was at the helm of the hotline project. Girls are married off at an early age and move in with their in-laws, often in another village, so they sever ties with their own families.
Once in their marital home “the new bride is expected to cook, clean and take care of her in-laws while also starting to think about procreating,” said Khan. “They do not have any agency.”
Kumari’s sister-in-law Anjali’s experience echoes Khan’s words: “Getting pregnant was not my decision,” she told CNN, adding that she felt societal pressure to get pregnant and did not have anyone to talk to about all this.
It is against this backdrop that Samya Mobile Baani was set up and because of the size of the need, it made an immediate impact.
So impactful was the work that Jha and the others were doing, that word spread to other villages. “Women who used the services also shared the number of the hotline to other women in different villages and they too called in,” said Khan.
Dr Prabha Chandra, head of perinatal mental health at the National Institutes of Mental Health and Neurosciences who was not involved with the hotline believes programs like this are valuable in addressing the burden of maternal mental health in the region because local people are trained to help others in their community. This is “important in a country like India where there are not enough psychiatrists,” she told CNN.
But funding only allowed the hotline to run for seven months as the rest of the one-year grant was needed to first develop the hotline and then write up the impact. Attempts to restart it through renewed funding were delayed as the Covid-19 pandemic diverted all attention and resources.
In the end though, says Dr Vijaya Raghavan, a psychiatrist with SCARF India, the sustainability of such initiatives is always threatened because they exist outside of national health policies and priorities. The only option, he believes, “is if these mental health projects are integrated into the country’s healthcare system.”
Raghavan also described how maternal mental health falls through the cracks because each individual symptom or risk factor can be attributed to a different root cause. “If we analyze anemia to be a triggering condition for perinatal depression and try to talk to the health department about the problems, they will say it is a nutrition problem and lead us to them. The nutrition department will say they have provided all nutritional sustenance and perhaps it is not reaching the women due to lack of education and lead us to the education department and that just goes on,” he said.
In the absence of the funded, staffed hotline, Jha and the others who were trained to offer peer-to-peer counseling continue to receive calls to their personal phones from women in the community, each as desperate as Kumari was for help or advice. Jha says she does what she can but is aware it is far from enough.
“When I met Kumari and Anjali, I sat and spoke with Anjali for a while, explained how eating is important for the baby, how she can always call me if need be. But that is all I could do,” she told CNN. “[Before] we had psychiatrists and counselors we could consult with when we ran into any severe case.”
Jha did also task Kumari with taking Anjali to the local hospital every other week for a checkup, so that at she is regularly attended to by a medical professional, even if they are not trained to handle mental health issues specifically.
Aware of the multiple responsibilities she herself carries, Jha is worried about how long she will be able to help the women who call her.
“I am burdened with all my other work, and I don’t know how long I can continue to support them without getting support,” she said. She leaves Anjali and Kumari, needing to get home to do the chores and knowing that whatever happens here, tomorrow will still be another busy day for her.
—-
If you or someone you know might be at risk of maternal mental health disorders, here are ways to help.
If you are in the US, you can call the PSI HelpLine at 1-800-944-4773 or text “Help” to 800-944-4773.
—-
Edited by Meera Senthilingam and Eliza Anyangwe.
.