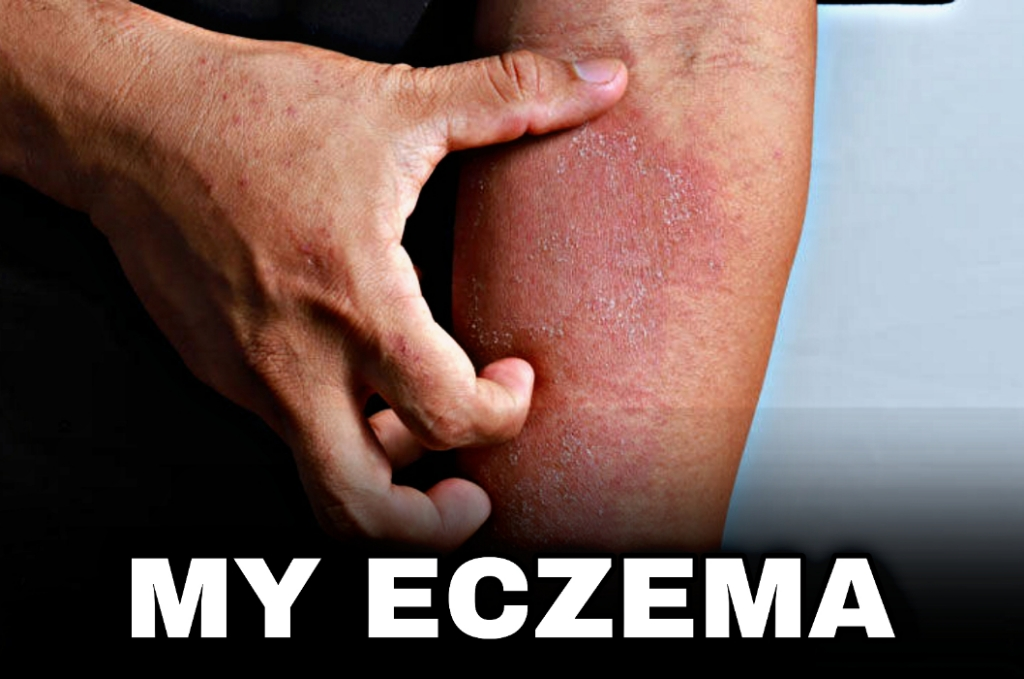
What is Causing My Eczema?
Eczema is a common skin condition that affects millions of people worldwide. It is characterized by dry, itchy, and inflamed skin. If you’re dealing with eczema, you might be wondering what is causing your symptoms and how you can find relief. In this comprehensive guide, we will explore the various factors that contribute to eczema and provide valuable insights on managing this condition effectively.
- What is Causing My Eczema?
- Understanding the Skin Barrier
- Common Risk Factors for Eczema
- Different Forms of Eczema
- Identifying Eczema Triggers
- Effective Strategies for Managing Eczema
- Conclusion
- FAQs
- Q: Do certain foods trigger eczema?
- Q: Is eczema contagious?
- Q: How is eczema diagnosed?
- Q: Who diagnoses eczema?
- Q: How do you treat childhood eczema?
- Q: What type of moisturizer treats eczema?
- Q: How soon after treatment will I feel better?
- Q: Are there complications from eczema?
- Q: What can I expect if I have eczema?
- Q: How long does eczema last?
- Q: Does the weather make eczema worse?
- Q: What questions should I ask my healthcare provider?
- Q: How do I take care of myself?
- Q: Which deficiency causes eczema?
- Q: How do you permanently treat eczema?
- Q: What causes eczema flare-ups?
- Q: What causes eczema in adults?
Understanding the Skin Barrier
The skin barrier plays a crucial role in maintaining healthy and moisturized skin. However, in individuals with eczema, this barrier becomes compromised, leading to increased water loss and susceptibility to irritants. The weakened skin barrier allows irritants to penetrate easily, triggering eczema symptoms. Understanding the importance of the skin barrier is the first step in managing and preventing eczema flare-ups.
Where do symptoms of eczema appear on my body?
Eczema can appear on various parts of the body, and the specific location may vary from person to person. The symptoms of eczema typically manifest as red, itchy, and inflamed patches of skin. Here are some common areas where eczema can occur:
- Face and Neck: Eczema can affect the cheeks, forehead, and around the eyes and mouth. The skin may appear red, dry, and flaky, and there may be a sensation of itchiness and discomfort.
- Hands: The hands are frequently affected by eczema, especially among individuals who frequently wash their hands or are exposed to irritants or allergens. The skin on the hands may become dry, cracked, and itchy, with the possibility of painful fissures.
- Elbows and Knees: Eczema patches often appear on the elbows and knees. These areas may develop thickened, scaly skin and experience intense itching. The constant bending and movement of these joints can further aggravate the condition.
- Behind the Knees and in the Elbow Creases: Eczema commonly occurs in the skin folds, such as behind the knees and in the creases of the elbows. The skin in these areas can become red, inflamed, and prone to irritation due to friction and moisture buildup.
- Scalp: Eczema can affect the scalp, resulting in itchiness, flaking, and redness. It may resemble dandruff or seborrheic dermatitis and can lead to discomfort and self-consciousness.
- Torso and Limbs: Eczema patches may appear on the chest, abdomen, back, arms, and legs. The affected skin can be dry, itchy, and irritated, often accompanied by redness and inflammation.
- Feet: Eczema can affect the feet, particularly the soles and sides. The skin may become dry, scaly, and prone to cracking. Itchy blisters may also develop, causing discomfort and difficulty in wearing shoes or walking.
Common Risk Factors for Eczema
While the exact cause of eczema remains unknown, certain risk factors have been identified that can increase an individual’s likelihood of developing the condition. These risk factors include:
- Genetics: Eczema tends to run in families, suggesting a genetic predisposition to the condition.
- Allergies: People with eczema often have other allergies, such as hay fever or asthma, indicating a possible connection between allergic reactions and eczema.
- Environmental Factors: Exposure to certain environmental triggers like dust mites, pet dander, and pollen can exacerbate eczema symptoms.
- Sensitive Skin: Individuals with naturally sensitive skin are more prone to developing eczema.
Different Forms of Eczema
Eczema is a broad term that encompasses various forms of the condition. Understanding the different types of eczema can help in identifying the specific triggers and managing the symptoms effectively. Some common types of eczema include:
- Atopic Dermatitis: This is the most prevalent form of eczema and is often seen in individuals with a family history of allergies or asthma.
- Contact Dermatitis: Contact with irritants or allergens can cause this form of eczema, resulting in localized inflammation and itching.
- Nummular Eczema: Characterized by coin-shaped patches of irritated skin, nummular eczema can be triggered by dry skin or exposure to irritants.
Identifying Eczema Triggers
Eczema triggers can vary from person to person, but there are some common factors that tend to irritate the skin and worsen symptoms. By identifying and avoiding these triggers, individuals with eczema can experience significant relief. Some common eczema triggers include:
- Dry Skin: When the skin lacks moisture, it becomes more susceptible to irritation and inflammation.
- Hot Water: Excessive exposure to hot water can strip the skin of its natural oils, leading to dryness and aggravation of eczema symptoms.
- Allergens: Substances like pollen, dust mites, pet dander, and certain foods can trigger allergic reactions, causing eczema flare-ups.
- Irritants: Harsh soaps, detergents, fragrances, and chemicals can irritate the skin and exacerbate eczema symptoms.
Effective Strategies for Managing Eczema
While there is no cure for eczema, several strategies can help manage the condition and prevent flare-ups. Here are some practical tips to incorporate into your daily routine:
- Moisturize Regularly: Keeping your skin well-hydrated is essential in managing eczema. Apply a thick, fragrance-free moisturizer immediately after bathing to lock in moisture. Reapply throughout the day, especially in dry or affected areas.
- Avoid Triggers: Take note of the factors that trigger your eczema flare-ups and make a conscious effort to avoid them. This may involve wearing gloves when handling irritants, using fragrance-free products, and keeping your home environment clean and dust-free.
- Identify Food Allergies: Some individuals with eczema may have food allergies that contribute to their symptoms. Consult with a healthcare professional to determine if certain foods are triggering your eczema and consider an elimination diet to identify and eliminate problem foods.
- Practice Gentle Skincare: Opt for gentle, hypoallergenic skincare products specifically formulated for sensitive skin. Avoid harsh scrubs, exfoliants, and abrasive materials that can further irritate your skin.
- Manage Stress: Stress can exacerbate eczema symptoms. Incorporate stress management techniques into your daily routine, such as meditation, deep breathing exercises, or engaging in activities you enjoy.
- Wear Breathable Fabrics: Choose clothing made from soft, breathable fabrics like cotton. Avoid wearing synthetic materials that can trap moisture and heat, leading to increased irritation.
- Keep Nails Short: Long nails can inadvertently scratch and damage the skin, worsening eczema symptoms. Trim your nails regularly and consider wearing gloves at night to prevent scratching during sleep.
- Use Mild Cleansers: Opt for gentle, fragrance-free cleansers that are specifically formulated for sensitive skin. Avoid harsh soaps or body washes that can strip away the natural oils and disrupt your skin’s barrier function.
- Consider Topical Steroids: In severe cases, a dermatologist may prescribe topical steroids to reduce inflammation and provide relief. It’s important to follow the instructions provided by your healthcare professional when using these medications.
- Consult with a Healthcare Professional: If your eczema symptoms persist or worsen despite your efforts, consult with a dermatologist or healthcare professional specializing in skin conditions. They can provide personalized advice and recommend appropriate treatment options.
Conclusion
By implementing these strategies and being mindful of your triggers, you can effectively manage your eczema and experience relief from its symptoms. Remember, consistency and patience are key in achieving long-term control over your condition.
FAQs
Q: Do certain foods trigger eczema?
A: For some individuals, certain foods can trigger or worsen eczema symptoms. Common culprits include dairy products, eggs, nuts, wheat, soy, and seafood. It’s advisable to keep a food diary and consult with a healthcare professional to identify and eliminate any potential food triggers.
Q: Is eczema contagious?
A: No, eczema is not contagious. It is a non-infectious condition that involves an overactive immune response and impaired skin barrier function. It cannot be transmitted from person to person through direct contact.
Q: How is eczema diagnosed?
A: Eczema is typically diagnosed through a combination of medical history, physical examination, and evaluation of symptoms. A healthcare professional, such as a dermatologist, will assess the appearance and location of the skin rash and inquire about any accompanying symptoms.
Q: Who diagnoses eczema?
A: Eczema can be diagnosed by various healthcare professionals, including dermatologists, pediatricians, allergists, or primary care physicians. They have the expertise to recognize the characteristic symptoms and patterns of eczema and provide appropriate diagnosis and treatment.
Q: How do you treat childhood eczema?
A: The treatment approach for childhood eczema often involves a combination of strategies. This may include gentle skincare practices, regular moisturization, avoiding triggers, identifying and managing food allergies, using topical corticosteroids or other prescribed medications, and providing emotional support to the child and their family.
Q: What type of moisturizer treats eczema?
A: When choosing a moisturizer for eczema, opt for a fragrance-free, hypoallergenic product that is specifically formulated for sensitive skin. Look for ingredients like ceramides, glycerin, and hyaluronic acid, which help restore and maintain the skin’s natural barrier function.
Q: How soon after treatment will I feel better?
A: The timeline for improvement varies from person to person and depends on the severity of eczema and the chosen treatment approach. Some individuals may experience relief within days or weeks, while others may require longer-term management to control symptoms effectively.
Q: Are there complications from eczema?
A: Eczema can lead to potential complications, such as skin infections, which can occur when bacteria enter through breaks in the skin caused by scratching. Additionally, the chronic itchiness and discomfort associated with eczema can have a negative impact on an individual’s quality of life, affecting sleep, daily activities, and emotional well-being.
Q: What can I expect if I have eczema?
A: If you have eczema, you can expect to experience recurring episodes of dry, itchy, and inflamed skin. The severity and frequency of flare-ups may vary, and it is essential to develop an individualized management plan in consultation with a healthcare professional.
Q: How long does eczema last?
A: Eczema is a chronic condition that can last for months or even years. It tends to follow a cycle of flare-ups and periods of remission. With proper management and treatment, the goal is to minimize flare-ups and maintain long-term control.
Q: Does the weather make eczema worse?
A: Extreme weather conditions, such as cold, dry winters or hot, humid summers, can potentially trigger or worsen eczema symptoms. It’s important to protect your skin from harsh weather by wearing appropriate clothing and using moisturizers to maintain hydration.
Q: What questions should I ask my healthcare provider?
- What type of eczema do I have, and what are its specific characteristics?
- What triggers are known to worsen my eczema symptoms, and how can I avoid them?
- Are there any specific tests or diagnostic procedures that can help identify underlying factors contributing to my eczema?
- What are the recommended treatment options for my eczema? Are there both topical and oral medications available?
- How long should I use the prescribed medications, and are there any potential side effects I should be aware of?
- Can you provide guidance on proper skincare routines and the use of moisturizers for managing my eczema?
- Are there any alternative or complementary therapies that may help alleviate my symptoms?
- Should I make any dietary changes to help manage my eczema? Are there specific foods or allergens I should avoid?
- Can you recommend any support groups or resources where I can connect with others living with eczema?
- What are the signs of a potential skin infection, and when should I seek medical attention?
Q: How do I take care of myself?
A: Taking care of yourself is crucial in managing eczema. Here are some self-care tips:
- Follow a regular skincare routine with gentle cleansers and moisturizers.
- Avoid scratching or rubbing the affected areas to prevent further irritation.
- Keep your skin well-hydrated by applying moisturizer regularly.
- Wear soft, breathable clothing made from natural fibers.
- Identify and avoid triggers that worsen your symptoms.
- Practice stress management techniques to reduce emotional stress.
- Maintain a healthy lifestyle with a balanced diet, regular exercise, and sufficient sleep.
Q: Which deficiency causes eczema?
A: While eczema is primarily driven by genetic and immune system factors, certain nutrient deficiencies may contribute to its development or aggravation. Deficiencies in essential fatty acids, such as omega-3 fatty acids, zinc, and vitamin D, have been associated with eczema. However, it’s important to note that addressing these deficiencies alone may not lead to a complete resolution of eczema symptoms.
Q: How do you permanently treat eczema?
A: Eczema is a chronic condition, and currently, there is no known cure for it. However, with proper management and treatment, you can control and reduce flare-ups, leading to long-term relief. Treatment options may include topical corticosteroids, moisturizers, immunomodulators, antihistamines, and other prescribed medications. It’s crucial to work closely with your healthcare provider to develop an individualized treatment plan.
Q: What causes eczema flare-ups?
A: Eczema flare-ups can be triggered by various factors, including:
- Irritants: Substances like soaps, detergents, perfumes, and certain fabrics can irritate the skin.
- Allergens: Common allergens include pet dander, pollen, mold, dust mites, and certain foods.
- Dry Skin: Low humidity levels and inadequate moisturization can lead to dry skin, triggering eczema.
- Stress: Emotional stress or anxiety can contribute to eczema flare-ups in some individuals.
- Temperature and Climate: Extreme temperatures, hot baths, or exposure to harsh weather conditions may worsen symptoms.
- Hormonal Changes: Hormonal fluctuations, such as those occurring during pregnancy or menstrual cycles, can impact eczema.
Q: What causes eczema in adults?
A: The exact cause of eczema in adults is not fully understood. It is believed to be a combination of genetic and environmental factors. Adults with a personal or family history of eczema, allergies, or asthma are more prone to developing eczema. Environmental triggers, such as irritants, allergens, stress, hormonal changes, and certain occupations involving frequent handwashing or exposure to chemicals, can contribute to eczema in adults.
Remember, eczema management is highly individualized, and it’s important to consult with a healthcare professional for accurate diagnosis, treatment options, and personalized care.